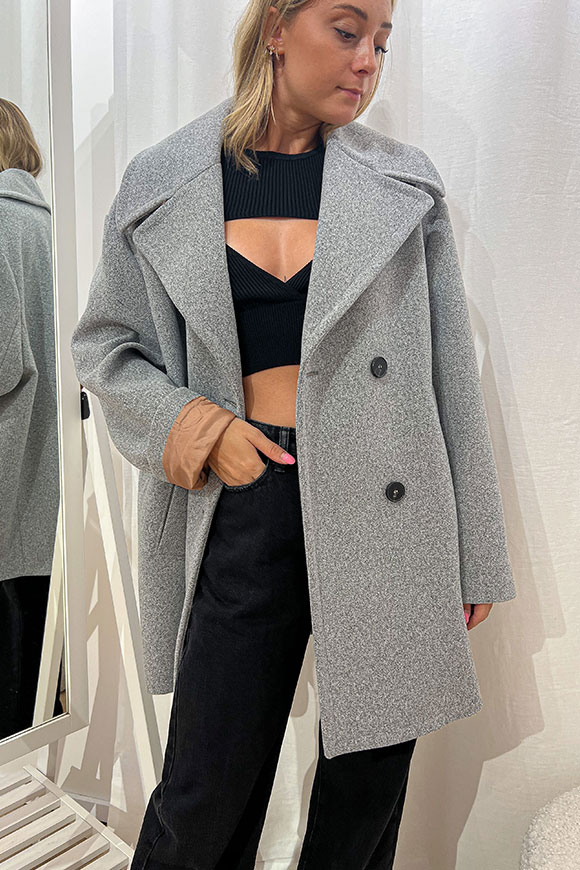
Cappotto uomo grigio spigato doppiopetto in lana rever largo made in italy - Carillo Moda | Abbigliamento uomo e donna, scarpe e accessori

ELEVENTY CAPPOTTO DOPPIOPETTO SPIGATO GRIGIO BIANCO, ELEVENTY CAPPOTTO INVERNALE UOMO, ELEVENTY SHOP ONLINE, CONTREBOUTIQUES. - Contre - i migliori brand di abbigliamento on-line